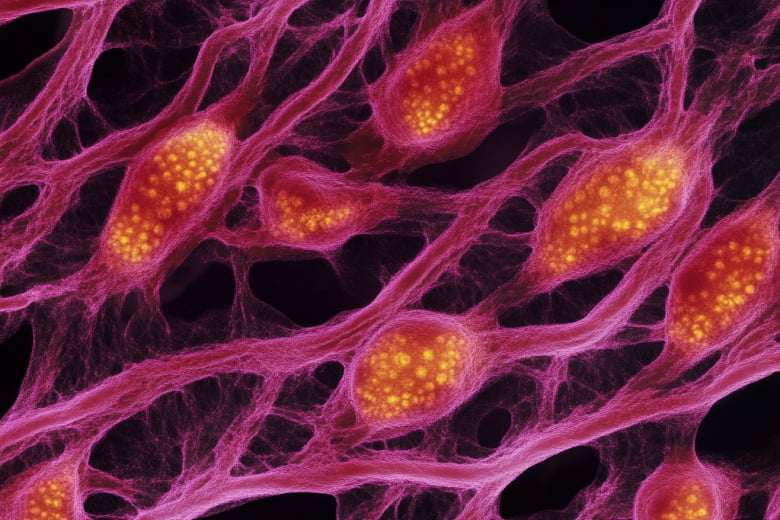
Skeletal muscle can be a highly regenerative environment,
allowing for the repair of injured muscle
fibers without scarring or long-term damage, however,
it is a complex process involving many different
cell types including myogenic and fibro-adipogenic
progenitor (FAP) cells in varying differentiation
states. The presence or absence of these cells, in their
varying states of differentiation, determine the effectiveness
of tissue repair. In addition to the presence
or absence of cells in the right differentiation state,
a complex array of factors play a role in successful
muscle regeneration including genetic predispositions
of the individual and the current environmental
state of the tissue such as the current disease state,
and the degree of injury.
The regenerative environment of muscle in healthy
individuals is typically stable; however, it can be
influenced by the degree of tissue damage and exhaustion
or reduction in progenitor cells. In certain
disease states, such as Duchenne Muscular Dystrophy
(DMD), the regenerative process goes awry and
progessive loss of regenerative function occurs.1 The
DMD phenotype arises due to mutations in the dystrophin
gene, resulting in no dystrophin production
or a lack of functional dystrophin protein. Dystrophin
is a critical structural protein found in skeletal
muscle and its absence results in severe muscular atrophy
and tissue loss. When functional dystrophin
is unavailable in the muscle fibers of DMD patients,
their muscles tear, break down, and undergo an endless
cycle of regeneration resulting in the eventual
deposition of fibrotic and fatty tissue with no muscle
function. Afflicted patients often become wheelchair-
bound before their teens and typically do not
survive beyond their late teens or early twenties.1
Beyond genetic disorders, a degenerative environment
can be produced through Volumetric Muscle
Loss (VML) injury.2 3 VML is caused by traumatic
or surgical loss of muscle tissue resulting in the development
of functional issues with the traumatized
muscle.4 This can commonly occur from gunshot
wounds, car accidents, or crush injuries. In the case
of VML injuries that involve 20% or more of the
muscle, the tissue is no longer able to self-repair, and
is instead burdened by fibrotic infiltration and associated
pathologic secondary conditions. This results
in further muscular degeneration, pain, stiffness,
and loss of funciton.5 6
In DMD and VML, the dysregulation of cell signaling
influences FAP cells, resulting in the deposition
of fatty and fibrotic tissue. FAP cells are muscle-resident
fibrogenic/adipogenic progenitor cells that
may play a role in regulating muscle healing. Interestingly,
FAPs do not appear to be important for the
development of skeletal muscle; however, a growing
body of evidence suggests that these cells may play a
critical role in appropriate healing following injury.7
Thus, the crosstalk between mature muscle, skeletal
muscle progenitor cells (skMDC), and FAP cells are
critical for proper muscle homeostasis and repair after
injury.
Get in touch
Complete this form and one of our product experts will connect with you shortly.
Investigators and study participants currently involved in one of the Cook MyoSite, Inc. clinical trials
should not
use this contact form.
If you are a study participant currently involved in one of the Cook MyoSite, Inc. clinical trials, please instead contact your treating physician.
If you are a study participant currently involved in one of the Cook MyoSite, Inc. clinical trials, please instead contact your treating physician.